How dilated am I?
16 June 2021
Planning where to give birth to your baby
17 June 2021
Birthing your Placenta
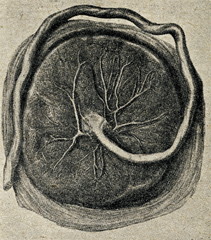
After you have birthed your baby, your next task is to birth your placenta! You can read more about the placenta in The Real Birth Company’s What’s What article, here. Birthing your placenta is often referred to as the third stage of labour, although it’s not a separate event or stage, it’s just a continuation of your baby’s birth.

What happens when I birth my placenta?
The good news is that the placenta is smaller and squishier than your baby, so it’s usually much easier to birth. You may feel it slip out shortly after your baby is born, or it may take a little longer.
Just before it arrives, or as it’s born, you’re likely to have a gush of blood from your vagina so don’t worry if you see that. It’s supposed to happen. If it’s more than normal your midwife will tell you.
I’ve been told about an injection to birth the placenta? What’s that about?
It is usually recommended that you have an injection of a drug which helps your uterus to shrink harder after birth, although the evidence of benefit is mixed. The drug is normally either Syntocinon, or, less often, a mixture of two drugs called Syntometrine. This is called having a managed, or active, third stage.
Syntocinon is an artificial form of the hormone oxytocin, and Syntometrine is a mixture of Syntocinon and another drug which makes the uterus shrink, Ergometrine. Ergometrine and Syntometrine may cause stronger contractions than Syntocinon, and it can therefore be a useful drug if a woman or person is bleeding heavily after birth, but it can cause unpleasant side effects including nausea and vomiting, or it can affect blood pressure, both of which can impact on a woman or birthing person’s ability to meet their new baby.
The drug is offered with the aim of reducing the chance of heavy blood loss at birth, although the evidence for this is poor. The Cochrane Review of the use of drugs to help to birth the placenta(1) concluded that using Syntocinon may reduce heavier than average blood loss, but it says that the evidence was “low quality”. It also says that there may be no difference between the numbers of women who needed a blood transfusion, whether or not they had Syntocinon.
If you decide to not have the injection, this is known as birthing your placenta physiologically.
What is controlled cord traction?
You are also likely to be offered controlled cord traction, which is where the midwife gently pulls on your cord while pressing on your abdomen once they have decided that the placenta has separated from your uterus. There is no good evidence that controlled cord traction is beneficial where Syntocinon is used and it can be painful(2). You can choose to have the injection without controlled cord traction if you prefer.
It is very important that no one pulls on your cord if you are birthing your placenta physiologically (without having the injection) as this can cause heavy bleeding.
How long does it take?
Most hospital guidelines say that the placenta should be born within 30 minutes if you have decided to have active management or an hour if you are birthing your placenta physiologically. These times are not based on good evidence.
If you are having a physiological placenta birth you may be asked to have the injection if you’ve not birthed your placenta within an hour. You don’t have to, the choice is yours. If you are having active management you may be told you need to have your placenta removed manually if it’s not birthed within half an hour, but again, you don’t have to. You may choose to, but if you are feeling well and there is no sign of bleeding you may feel more comfortable in waiting longer.

Can I do anything to help my placenta to be birthed?
Yes! The most important thing is to ensure that you keep the levels of your body’s oxytocin as high as possible. Oxytocin is the hormone which helps to shrink your uterus and helps your placenta to birth. Oxytocin can be boosted by keeping the lights low, asking people around you to speak softly and kindly, and by loving touch. Holding your baby skin to skin, smelling them (you can take their hat off if you want!), touching them, this all boosts your oxytocin. If you are feeling cold or shivery, say so, so that someone can cover you and warm you. Feeling warm, safe and cosy helps your oxytocin.
Changing position can help. If you’re sitting or lying down, and if you’re able to, try to stand, kneel forward or squat. Perhaps your birth partners can help you into these positions?
Sitting on the toilet can be a great way to release the placenta and it has the added benefit that it can help you to wee. Try running the tap to help this along! A full bladder can stop the placenta coming out so if you haven’t passed urine for a while your midwife can feel your belly to see if your bladder is full. This can be helpful even if you don’t feel that you need to wee because we often lose the urge for a short while just after birth, even if our bladder is really full. If your bladder is full and you can’t wee, your midwife can quickly release the urine with a catheter which is a tiny tube that is passed into your urethra and allows the urine to drain. This then makes the bladder much smaller and gets it out of the way of the placenta.
In Summary
Birthing your placenta is the final part of birthing your baby. It is often highly medicalised with the aim of reducing heavy blood loss, but the evidence for this is poor.
As with any intervention, you can decide whether or not you want to accept or decline it. Whether or not you accept active management of your placenta’s birth there are a number of things which you can do to help it to be birthed, and that those around you can help with too, so you may wish to consider including birthing your placenta on your birth plan.
References:
1) Cochrane Review: Prophylactic oxytocin for the third stage of labour to prevent postpartum haemorrhage: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD001808.pub3/full
2) Cochrane Review: Controlled cord traction for the third stage of labour: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD008020.pub2/full