RealBirth’s Digital Antenatal Programme Delivers Measurable Impact
6 August 2025
Bleeding after birth: understanding post-birth bleeding.
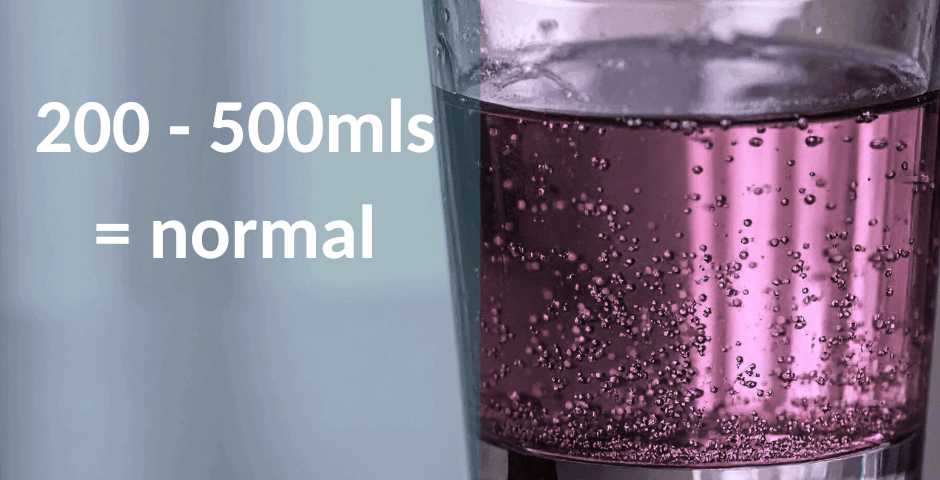
After giving birth, most women will experience some bleeding when the placenta comes away from the uterus. This is completely normal and is usually heavier than a typical period, for most people it will be between 200 – 500 mls of blood, a fizzy drink can is 330mls. This blood loss is part of keeping the body balanced, you do not need this blood anymore as you have given birth,
Once your baby is born, your uterus starts to shrink back to its pre-pregnancy size. As it does this, the placenta comes away naturally, and the blood from that area is released – often quite quickly. This is part of the normal healing process after birth.
You can learn more about this stage of labour, and why bleeding after birth is expected, during your Real Birth course – whether you're attending in person or online.
For some women they experience unexpectedly heavy bleeding—more than a heavy period—known as postpartum haemorrhage (PPH). Though it's less common, when it happens it needs quick support and management. This article explains how often this occurs in UK births, why starting labour early (induction of labour) increases the risk, and highlights how the Real Birth programme in Epsom and St Helier NHS Hospital helped reduce cases.

How common is heavy postpartum bleeding?
A UK-wide review of births in midwife-run centres found that about 3.7% of women required transfer to hospital care because of heavy bleeding after birth. A national study (“Birthplace”) previously showed around 1% for low-risk births needing transfer (PLOS). Severe bleeding happening in high-income countries rose around 5% per year between 2011–24 but it is thought that better training and awareness of PPH partly explains this increase, however there was also an increase in Induction of Labour in this time too.
Heavy bleeding mainly happens because the muscles of your uterus don’t tighten quickly after birth, especially if they are stretched a lot or injured, for example a twin birth may mean that the uterus is stretched to a slightly larger capacity or in a caesarean birth, cutting through the muscles layers prevents the womb from shrinking in the way it should do naturally. Emergency factors can also increase the chance, these include womb fatigue (atony, where the muscles have been working for an extended period of time), wounds from cutting the fibres, pressure on the placenta from pre-eclampsia, or blood clotting issues (Yunas, Idnan et al.)

Why starting labour early can raise risk
Research shows that low-risk pregnancies have a higher chance of postpartum bleeding if labour is medically started or sped up if labour has started naturally, compared to waiting for natural labour and progress to happen. In particular, the process of induction can be longer making the muscles of the womb tired, this makes them harder to shrink back to the size needed to prevent bleeding more than normal. Women with anaemia face greater risk if their labour is induced or sped up without a clear reason that truly indicates induction is best plan of care. (University of Oxford)
A 2019 UK study found that routine induction of labour in first time mothers increased the chance of PPH by 20%, for other people it didn’t increase average overall bleeding after birth—but it still remains a concern when other risk factors are present.
How education can reduce bleeding
At Epsom and St Helier NHS Trust Real Birth was evaluated for a year, the Real Birth programme emphasised techniques to help the womb shrink and tighten after birth: this included immediate skin to skin in all birth scenarios for example vaginal or caesarean birth, early initiation of feeding straight after birth to help the uterus to shrink more quickly naturally. Both techniques increase the release of oxytocin which helps the uterus to shrink, we also shared breathing techniques and upright positions to help the placenta birth. The evaluation showed a marked reduction in the PPH rates among Real Birth users.
Things to think about.
- Support iron levels: having good iron stores helps reduce the chance of bleeding and also improves your health if you did have a larger blood loss.
- Support womb tightening: After birth, immediate skin-to-skin contact, gentle movement, and upright positions help,
- Think about planned induction of labour for a term healthy pregnancy: Question the benefits and risk, for example is waiting for a bit longer if you are medically well better v’s possible increased bleeding risk, which will cause ill health.
- Prepare with education: Knowing how to support your body after birth makes a real difference.
Conclusion
Heavy bleeding affects around 3–4 in 100 UK births and starting labour early can raise this risk—especially if you're anaemic. The Real Birth Complete programme’s hands-on education helped reduce cases in the UK. Understanding your chance, the process, supporting birthing the placenta and aftercare can make a real difference.
References
Hall, J., Smith, L., Green, K., & Turner, H., 2023. Rates of postpartum bleeding in UK midwife-led units: A national review. PLOS One, [online] Available at: PLOS One.
National Perinatal Epidemiology Unit (NPEU), 2011. Birthplace in England Research Programme: Perinatal and maternal outcomes by planned place of birth. Oxford: NPEU. (Data collected 2008–2010).
Royal College of Obstetricians and Gynaecologists (RCOG), 2024. Trends in severe postpartum haemorrhage in the UK: A longitudinal analysis 2011–2024. The Lancet.
Taylor, R., Jennings, P., & Owens, H., 2025. Understanding the causes of postpartum haemorrhage: A national review. The Lancet.
National Perinatal Epidemiology Unit (NPEU), 2024. Risk factors for postpartum haemorrhage in induced labour: The role of maternal anaemia. University of Oxford.
Roberts, A., Bennett, J., & Evans, L., 2019. Early UK study on induction of labour and postpartum blood loss: A population-based analysis. British Journal of Midwifery.