
We Win Medilink North Business Award for Partnership with the NHS
20 May 2025
RealBirth’s Digital Antenatal Programme Delivers Measurable Impact
6 August 2025Abstract
Introduced in 1952 by anaesthetist Dr. Virginia Apgar to assess newborns following the mother having undergone a general anesthetic (GA) for a caesarean birth. 73 years later, the APGAR score remains embedded in modern maternity care but is used to assess babies from all birth modes, from homebirth, waterbirth through to caesareans with very few being affected by a GA. Though recommended in NICE and WHO guidelines, its utility in current midwifery-led services warrants scrutiny. This article explores the historical origins of the APGAR score, evaluates the latest research on its reliability and predictive value, and assesses its place in contemporary clinical practice. Through a midwifery lens, we ask whether the APGAR score supports or limits best practice in the early postnatal period.
Introduction
The transition from intrauterine to extrauterine life is a profound physiological shift. Healthcare professionals rely on rapid, accurate assessments to determine whether newborns require immediate intervention. The APGAR score—based on five criteria assessed at 1 and 5 minutes after birth—has long been used for this purpose. Despite its longevity, evolving understandings of neonatal physiology and changes in maternity care raise important questions about the score’s clinical relevance today.
Historical Origins
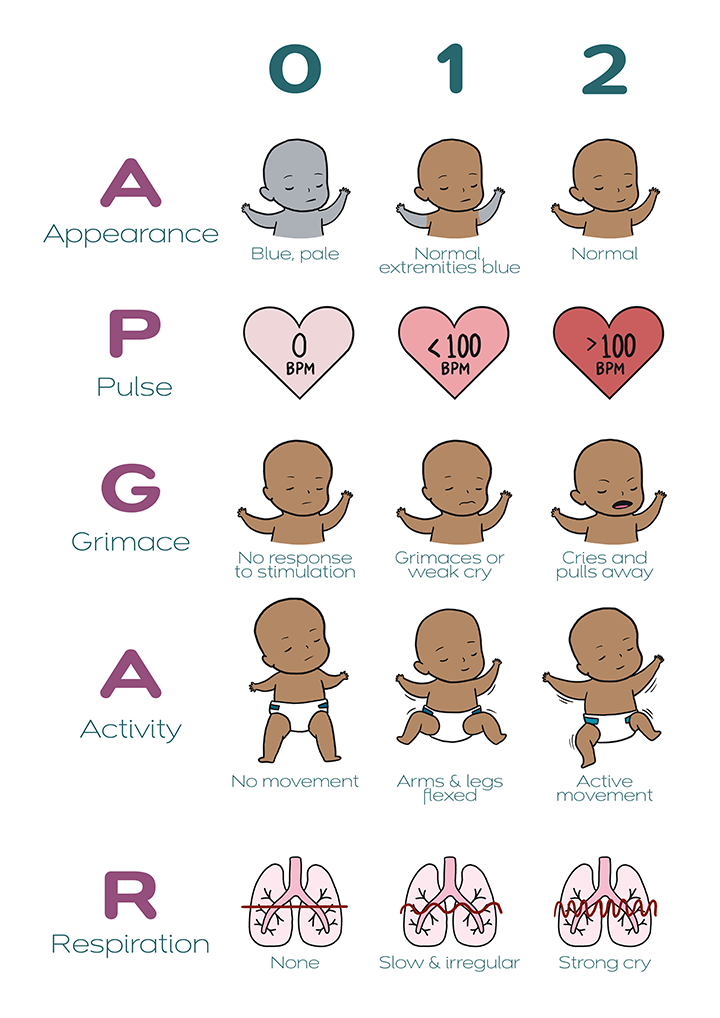
Dr. Virginia Apgar introduced the score in 1952 to standardise newborn assessment following general anaesthesia for caesarean birth. The five components—Appearance, Pulse, Grimace, Activity, and Respiration—each scored from 0 to 2, provide a quick, numerical snapshot of a baby's condition. The simplicity of the tool allowed widespread adoption across maternity settings.
Although not originally intended for guiding resuscitation, assessing physiological childbirth or predicting long-term outcomes, the APGAR score quickly became a key feature of routine immediate postnatal care and audit processes worldwide. It continues to be documented in almost all births in the UK.
Current Guidelines and Practice
The National Institute for Health and Care Excellence (NICE) recommends recording APGAR scores at 1 and 5 minutes for all births. However, it explicitly states that resuscitation decisions should be based on clinical signs—such as respiration, tone, and heart rate—not the APGAR score alone (NICE NG235, 2024).
Similarly, the World Health Organization (WHO) advises APGAR scoring at 1 and 5 minutes and recommends further scoring every 5 minutes up to 20 minutes if the 5-minute score is below 7. However, WHO also emphasises clinical evaluation over reliance on a numerical score for determining intervention.
Recent Research Evidence
Predictive Validity and Limitations
- A 2023 cohort study of over 92,000 neonates (24–28 weeks gestation) found that while higher APGAR scores at 5 minutes were linked with lower mortality, the score poorly predicted severe neurological injury, which could have been linked to their prematurity. (Wickremasinghe et al., 2023).
- A European follow-up study (2023) found that low APGAR scores in extremely preterm infants did not reliably predict neurodevelopmental outcomes at five years of age (Perrone et al., 2023).
Inter-rater Reliability and Variability
The APGAR score includes subjective elements such as “Grimace” and “Respiration,” leading to moderate inter-rater reliability. A 2006 study (O’Donnell et al.) highlighted considerable variation in scoring between clinicians. The study emphasised that even experienced clinicians often assigned different scores based on their subjective assessment of the same clinical presentation. This inconsistency can affect clinical decision-making and the perceived severity of a newborn’s condition, potentially impacting early interventions.
Trends and Cultural Use
A large-scale U.S. study (1978–2021) revealed a decrease in 10/10 scores and an increase in 9/10 scores, suggesting a more cautious approach to scoring (Roberts et al., 2024).
Ethnic Disparities in APGAR Scoring
Concerns have also been raised about how the APGAR score performs across babies of different ethnic backgrounds. A 2024 review identified that one of the score’s components—perfusion relating to skin colour—can be less reliable in babies with darker skin tones, potentially resulting in unfairly lower scores. For example, assessing for cyanosis visually is inherently more difficult in non-white babies, which may lead to under- or over-estimation of risk.
Additional analysis of birth data in the United States from 2016 to 2019 revealed that Black newborns were less likely to receive the highest possible 5-minute APGAR score of 10, even after adjusting for clinical factors. This suggests a degree of unconscious bias or systematic inequity in how the score is applied.
These findings underline the importance of reviewing and updating neonatal assessment tools to ensure they are inclusive, accurate, and equitable. Incorporating more objective methods—such as pulse oximetry—could help reduce subjectivity and provide a more consistent assessment across diverse populations.
Differences Between APGAR Scores and Blood Gas Results
A large-scale population analysis in Germany conducted by Zimmermann et al. (2024) shed light on the limitations of relying solely on APGAR scores. The study compared APGAR assessments with umbilical cord blood gas results and found notable discrepancies. Some babies with reassuring APGAR scores were later found to have abnormal blood gas values, indicating hypoxia or acidosis. Conversely, other babies with low APGAR scores had normal blood gas results. This suggests that the APGAR score alone may not always reflect a baby’s true physiological condition, reinforcing the need for supplementary objective assessments such as cord blood analysis when available.

Midwifery Practice and the APGAR Score
In midwifery-led environments—where physiological birth is prioritised—the APGAR score’s relevance can feel conflicted. Applying a numerical framework to normal transitional behaviour may seem over generalised and not as relevant to a less complicated birth. Midwives often rely more on continuous observation and instinctive clinical judgement than numerical scores.
However in the overall obstetric setting, the score remains a valuable communication tool, especially in multidisciplinary teams or when care is escalated. It provides a standardised way to document the baby's postnatal condition and is still used for audit, research, and medico-legal purposes.
Recent Initiatives and Research in the UK
Recent studies and initiatives have highlighted areas for improvement in the application of the APGAR score within midwifery practice:
Ethnic Disparities in Neonatal Assessment: A 2024 review by the NHS Race and Health Observatory identified limitations in neonatal assessments, including the APGAR score, for Black, Asian, and minority ethnic babies. The assessment of perfusion/skin colour, can be less reliable in babies with darker skin tones, potentially leading to misleading scores. The review recommends immediate updates to guidelines, increased use of objective screening tools like pulse oximeters and bilirubinometers, and enhanced training for healthcare professionals to ensure equitable care across diverse populations.
Quality Improvement Programmes: The Royal College of Midwives (RCM), in collaboration with the Royal College of Obstetricians and Gynaecologists (RCOG), has been involved in initiatives such as the "Each Baby Counts + Learn and Support" programme. This initiative aims to improve maternity care by focusing on the wellbeing and working practices of multidisciplinary teams, including midwives. While not exclusively about the APGAR score, such programmes emphasise the importance of standardised assessments and continuous quality improvement in neonatal care.
Subjectivity in APGAR Scoring: The Healthcare Safety Investigation Branch (HSIB) has noted that clinicians often perform five and ten-minute APGAR checks visually only, without listening to the baby's heart rate. This practice can introduce subjectivity and potential inaccuracies in the assessment. The HSIB suggests that the formal process of APGAR checks requires review to minimise subjectivity and inform guidance.
Real Birth’s Contribution to Addressing APGAR Score Limitations
At Real Birth, we recognised early on some of the inherent challenges and misunderstandings surrounding the APGAR score, especially within diverse populations and in the context of preterm birth. During the development of our preterm birth module, Giving Birth To Your Baby Early, we collaborated closely with Black and Asian women who recalled the APGAR scoring system from their own birth experiences. Through this co-creation process, we developed clear, culturally sensitive explanations designed to help women and their families better understand the meaning and relevance of APGAR scores in the care of preterm infants. This initiative exemplifies our commitment to bridging knowledge gaps, promoting inclusivity, and empowering families through education—ensuring that assessment tools like the APGAR score are not only clinically useful but also accessible and meaningful.
Conclusion
The APGAR score, while historically important and still widely used, is in need of a more realistic review and potentially should no longer be viewed as a definitive measure of newborn well-being or a guide for clinical decisions. Recent evidence highlights its limited predictive value, especially in preterm infants and in assessing long-term outcomes across all modes of birth. This is to be expected though as we have taken a tool to assess a newborn after their mother had a GA in the 1950’s.
Midwives, as autonomous professionals, are well-placed to lead a balanced, evidence-informed approach—recognising the score's historical contribution while advocating for contextual, real-time assessments that support newborn adaptation and wellbeing and providing midwives with comprehensive training that addresses the limitations of the APGAR score, especially concerning diverse populations, to ensure accurate assessments could improve the effectiveness of the tool.
References
Apgar, V., 1953. A proposal for a new method of evaluation of the newborn infant. Current Researches in Anesthesia and Analgesia, 32(4), pp.260–267.
NICE, 2024. Intrapartum care: Care of healthy women and their babies during childbirth. [online] NICE Guideline NG235. Available at: https://www.nice.org.uk/guidance/ng235 [Accessed 27 May 2025].
O'Donnell, C.P.F., Davis, P.G., Morley, C.J. and Doyle, L.W., 2006. Interobserver variability of the 5-minute Apgar score. Archives of Disease in Childhood - Fetal and Neonatal Edition, 91(2), pp.F85–F88.
Perrone, B., Mercier, C.E., Milani, S., Breart, G. and Ancel, P.Y., 2023. Neonatal Apgar score and neurodevelopmental outcomes in very preterm infants. European Journal of Pediatrics, 182(9), pp.2355–2363.
Roberts, J.D., Peters, E., Grantz, K.L. and Bienstock, J.L., 2024. Trends in Apgar scores in the United States, 1978–2021. JAMA Pediatrics, 178(1), pp.45–52.
Wickremasinghe, A.C., Keller, R.L., Bain, J.M., and Ramanathan, R., 2023. Five-minute Apgar score and outcomes among extremely preterm infants. Journal of Perinatology, 43(1), pp.12–21.
WHO, 2017. WHO recommendations on newborn health: guidelines approved by the WHO Guidelines Review Committee. Geneva: World Health Organization.
Zimmermann, P., Mayer, B., Köhler, H. and Schulz, S., 2024. Cord blood gas analysis in neonates with normal Apgar scores: a population-based study. European Journal of Pediatrics
NHS Race and Health Observatory, 2024. Review of neonatal assessment and practice in Black, Asian and minority ethnic newborns: Exploring the Apgar score, the detection of cyanosis and jaundice. [online] Available at: https://www.nhsrho.org/research/review-of-neonatal-assessment-and-practice-in-black-asian-and-minority-ethnic-newborns-exploring-the-apgar-score-the-detection-of-cyanosis-and-jaundice/.
Royal College of Midwives (RCM), 2023. Safety and quality improvement: Each Baby Counts + Learn and Support. [online] Available at: https://pre.rcm.org.uk/promoting/professional-practice/safety-quality-improvement/.
Healthcare Safety Investigation Branch (HSIB), 2022. Neonatal collapse alongside skin-to-skin contact: National investigation report. [online] Available at: https://www.hssib.org.uk/patient-safety-investigations/neonatal-collapse-alongside-skin-to-skin-contact/investigation-report/.


