
Empowering Antenatal Support: Real Birth Training in Sure Start Projects
25 June 2024
Sepsis Awareness Month
13 September 2024This year the RealBirth Company is working hard to tackle the topic of induction rates on the rise, it is important that women and birthing people fully understand the process and any possible implications that could affect themselves or their babies, to truly make informed decisions about their care. January 2025 will see the launch of a new induction of labour module within the Real Birth Workshop.
Earlier in the year we discussed the rising rate of labour inductions in the context of the ongoing maternity staffing crisis. There is no doubt that the increasing induction rate and increasing complexities in modern maternity care are impacting the workload, and potentially having unintended consequences on already pressured services.
Another potential concern is whether the increased use of various labour and birth interventions, specifically the use of artificial oxytocin used for induction of labour or augmentation, are having an unintended effect on breastfeeding rates and women’s experiences of breastfeeding.
Is it possible that increased use of interventions in labour are making it harder for women and birthing people to breastfeed their babies? Is there a correlation between interventions and rates of breastfeeding?
Research has suggested that a number of common maternity interventions could have a negative impact on breastfeeding. These include:
● Epidurals
● Induction of labour
● Augmentation of labour
● IV fluids
● Assisted vaginal births
● Elective (pre-labour) caesarean births
● Separation of mother and baby
Within this article we will explore induction of labour and the use of artificial oxytocin for induction and augmentation of labour, and the possible correlation between increased induction rates and lower rates of breastfeeding.
————————————
Medical intervention within maternity care, and the availability of prompt medical assistance can be beneficial in select circumstances, however, it is important to consider the possible wider implications of such widespread practices – especially in circumstances where they may not always be clinically indicated.
How does induction impact breastfeeding?
You may be wondering how a labour intervention such as induction and use of synthetic oxytocin, could impact breastfeeding experiences, given that oxytocin is the very hormone needed for successful breastfeeding. But we must acknowledge that childbirth exists along a physiological continuum. It would be naive to assume that something we do on one end of the continuum, could not possibly impact events on the other end of the continuum.
Medically, birth and breastfeeding are generally considered two completely separate events, but evidence demonstrates that how we give birth can affect how our baby latches to the breast. We must acknowledge that the choices made in labour can both enhance or deter a mother’s ability to be able to successfully breastfeed her baby. Despite decades of research, this remains an understudied, and misunderstood area of our physiology.
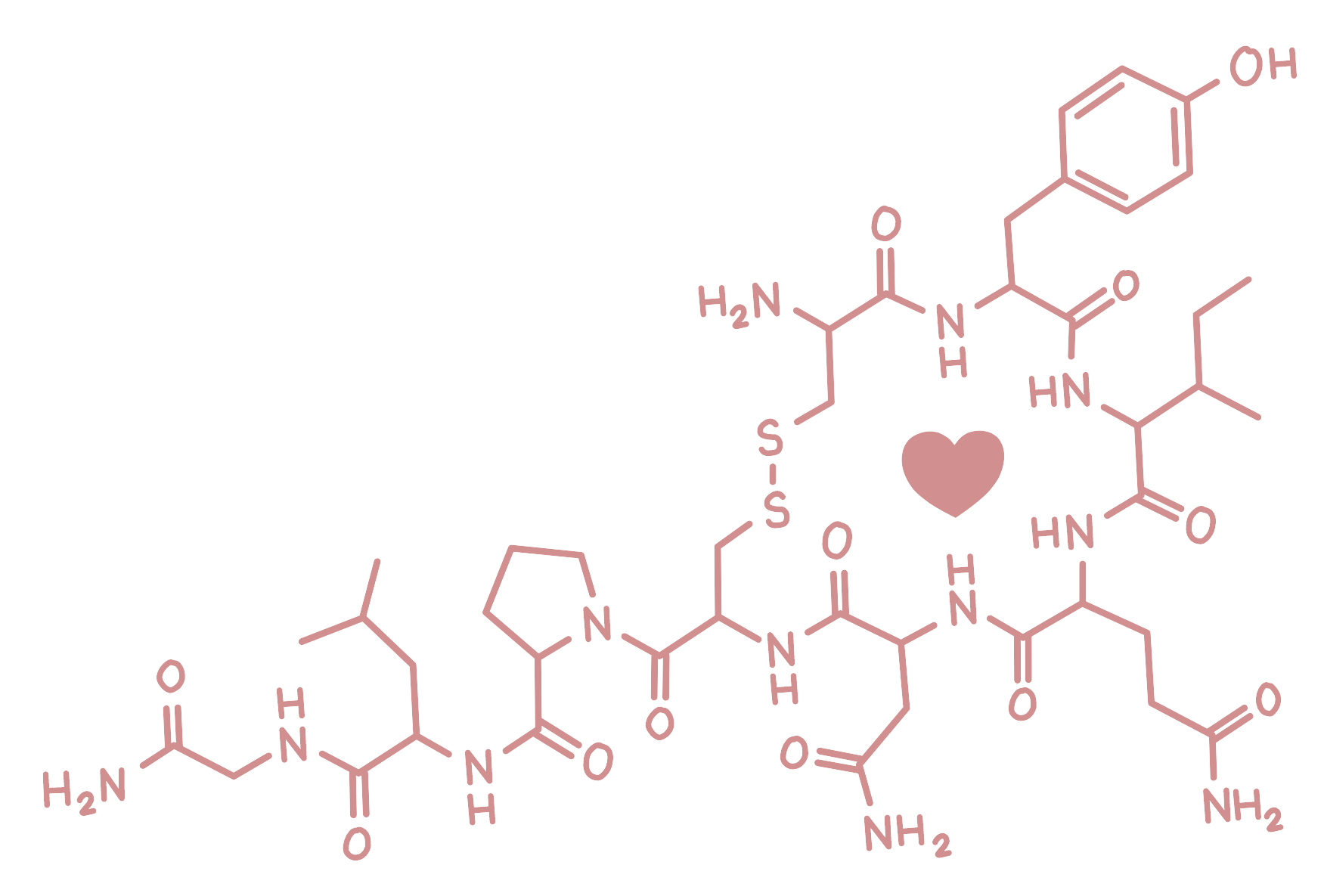
To truly understand the impact of induction of labour on breastfeeding, we must fully understand the role and function of oxytocin (and other birthing hormones), and the differences between endogenous (naturally produced) oxytocin and synthetic oxytocin. We must also understand the many physiological processes that support successful breastfeeding, and how they may differ under the influence of synthetic oxytocin.
Breastfeeding physiology
Oxytocin
Oxytocin receptors can be found in the smooth muscle fibres of the uterus and the breasts, and are laid down towards the end of pregnancy. Our central nervous system, including the spine and the brain, also contain oxytocin receptors thought to be responsible for facilitating social learning, memory consolidation and bonding.
Oxytocin also reduces stress by activating the parasympathetic nervous system, which promotes calm, connection, healing, and growth; and by reducing activity in the sympathetic nervous system, which reduces fear, stress, and stress hormones.
Levels of oxytocin rise throughout labour, and soar immediately after birth. As the baby passes through the birth canal, stretch receptors in the vagina trigger a final surge of oxytocin, meaning levels are extremely high for both the mother and the baby immediately after birth. The initial period after a physiological birth is highly sensitive. Skin to skin time with our baby also triggers further release of oxytocin, making our body perfectly primed for breastfeeding.
Peak oxytocin levels also promote a number of other benefits including;
● Helping to shrink the uterus after birth to reducing the chance of postpartum haemorrhage
● Natural warming for the baby through vasodilation of mother’s chest
● Activation of hormonally-mediated mother-baby bonding
● Reduction in maternal and newborn stress.
Although a completely natural function, successful breastfeeding is a complex biological process involving different hormones and the mother baby dyad working together in synchronicity.
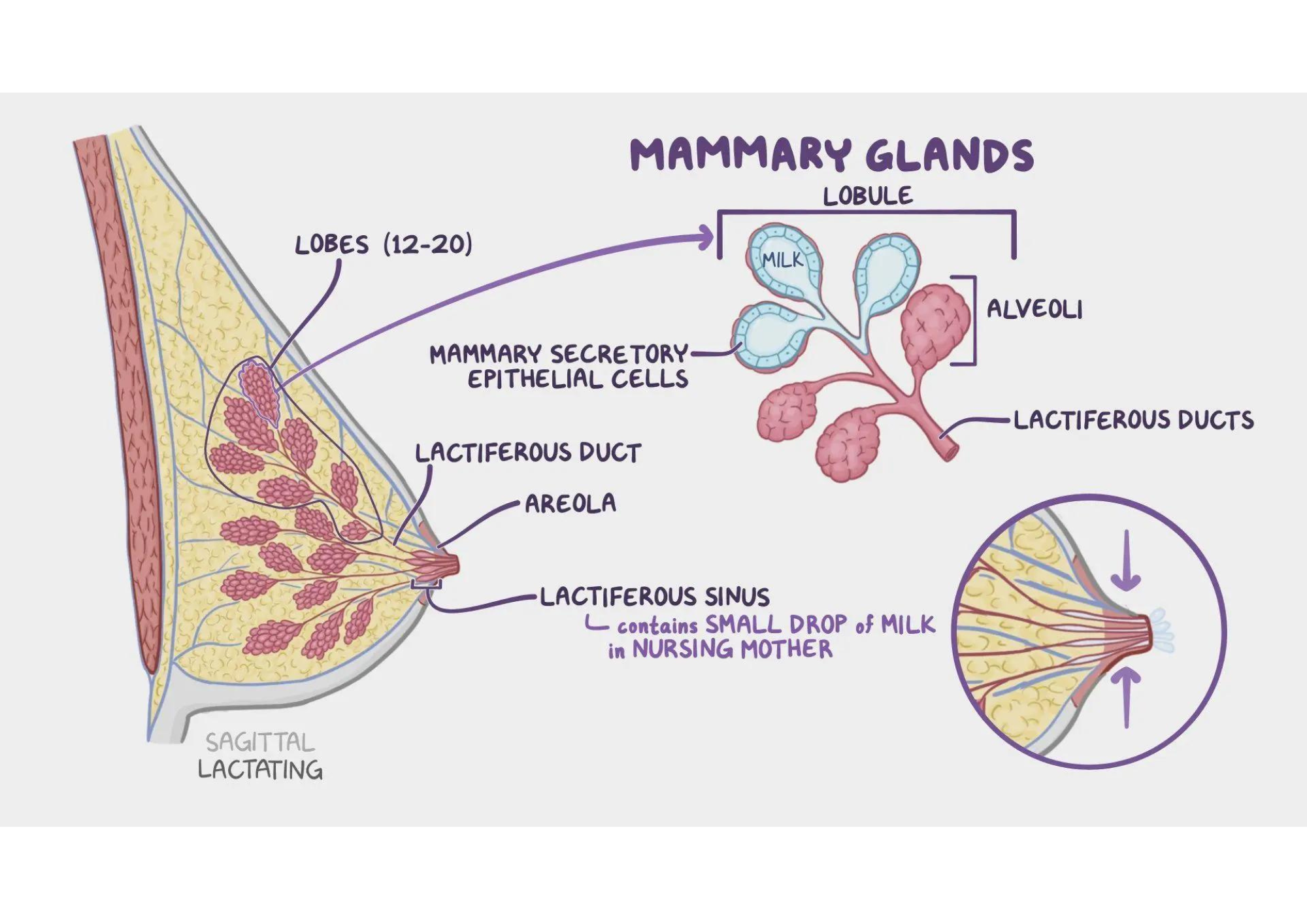
As the baby suckles at the breast, the tactile stimulation triggers the pulsatile release of oxytocin from the posterior pituitary gland. Circulating oxytocin causes the smooth muscle cells within the alveoli of the breast to contract, pushing milk into the milk ducts. The ducts act as a temporary store until the milk is removed by the baby. As the baby continues to suckle, the wave-like action of their tongue compresses the breast tissue against the hard palate of their mouth releasing the milk from ducts, and out through the nipple where it is swallowed. This is known as milk ejection or the ‘let-down’ reflex.
Once lactation is established, it is maintained by a combination of physical and hormonal factors. If milk is not removed from the breast regularly, pressure builds up within the breast causing an inhibitory feedback factor which reduces the production of milk. If breast milk is removed, then the inhibitory factor is also removed, creating the opposite effect. This regulates the amount of milk produced, which is determined by how much the baby takes and needs. In simple terms, the more milk is removed, the more milk the body will continue to make. If less milk is removed, the body will assume the baby does not need as much, and therefore will produce less to prevent the breasts from getting engorged.
Lactation and breastfeeding can be negatively affected by anything that interrupts these physical and hormonal processes.
Prolactin
Prolactin is another important hormone when it comes to breastfeeding. Prolactin is responsible for the physiological breast changes that occur during pregnancy. It stimulates the growth of the alveoli where breast milk is produced.
Prolactin levels rise throughout pregnancy and are elevated significantly in late pregnancy, helping with the formation of prolactin receptors in the brain and the breasts. Prolactin levels rise steeply as birth approaches, likely due to peaks in beta endorphins and oxytocin – both of which stimulate prolactin release.
For the baby, prolactin levels also rise towards the physiological onset of labour, and may assist in the physiological transitions they must go through after birth. Prolactin present in the amniotic fluid fills the fetal lungs, and may play a beneficial role in preparing them for extrauterine life and respiratory adaptations.
Prolactin levels remain high for several hours after birth and may promote breast milk production and maternal adaptations. It is thought that prolactin released during early and frequent breastfeeding is linked to maternal adaptations including reducing anxiety, aggression, muscle tension as well as social desirability, which may help mothers to prioritise newborn care.
Differences between natural and synthetic oxytocin
The association between synthetic oxytocin and uterine hyperstimulation is well known. Hyperstimulation is defined as more than 5 labour tightenings in 10 minutes, for 2 consecutive 10 minute periods. Synthetic oxytocin is structurally identical to natural oxytocin, so when oxytocin receptors are occupied by either synthetic or natural oxytocin, labour tightenings will result.
As natural oxytocin is released in pulses, compared to the continuous administration of synthetic oxytocin via a drip, in physiological labour the smooth muscle cells of the uterus have time to recover in between pulses. When synthetic oxytocin is administered in high doses, or for extended periods, the muscle cells cannot recover in the same way.
During physiological labour, the intermittent decrease of blood flow to the placenta at the peak of a labour tightening is usually well tolerated by a healthy term baby. However, during induced labours, we know that synthetic oxytocin brings about longer, stronger, more intense labour tightenings which are less well tolerated by the baby, increasing the likelihood of fetal hypoxia, acidosis and poor Apgar scores at birth.
Hyperstimulation during induced labour is not uncommon. One study documented that 30.2% of induced labours resulted in hyperstimulation, with the same applying to labours augmented with synthetic oxytocin also. The greater number of labour tightenings experienced in a 30 minute period resulted in greater negative effects on the baby and increased neonatal morbidity.
With this in mind, it is easy to see why babies exposed to synthetic oxytocin in labour, have a greater chance of being admitted to the neonatal unit, resulting in a likely separation from their mother in the initial postpartum period and missed opportunities for skin to skin and breastfeeding.
Synthetic oxytocin and breastfeeding
Research has suggested that the administration of synthetic oxytocin in labour may impact breastfeeding in a number of possible ways:
- Interruptions to the maternal oxytocin system – reducing natural oxytocin
- Increased chance of adverse neonatal outcomes – increasing likelihood of maternal newborn separation
- Altered breastfeeding behaviours in the newborn.
Synthetic oxytocin is thought to inhibit the action of maternal oxytocin in the immediate postpartum period. This occurs through desensitisation of oxytocin receptors, inhibiting the mother’s own oxytocin release. This response was found to be dose dependent, meaning that women who’d received the highest doses of synthetic oxytocin in labour, released the lowest amounts of their own oxytocin.
Synthetic oxytocin has been found to cross the placenta and the immature blood/brain barrier of the baby during labour, and desensitises the infant’s oxytocin receptors within the central nervous system, affecting their function.
Researchers found that babies exposed to synthetic oxytocin in labour were 11.5 times more likely to show lower levels of feeding cues, compared to babies who were not exposed.
Other research has shown that babies exposed to synthetic oxytocin in labour, showed a significant reduction in primitive reflexes associated with breastfeeding, and that these results were not dose dependent.
The 9 instinctive stages that newborns display during immediate skin to skin after birth have been well documented. They were first described by Widstrӧm in 1987. These stages are evolutionarily necessary for newborn survival during the first hour of birth and beyond.
- Birth cry – inflates the lungs for the first time. This is a newborn’s innate survival instinct
- Relaxation – occurs after the birth cry ends. The baby shows no visible movements
- Awakening – the baby shows small movements of the upper body – head, shoulders and movements of the mouth
- Activity – the baby now shows larger body movements including lifting the head, rooting behaviours and hand-breast-mouth movements
- Resting – this can happen at any point within the first hour, and can be interspersed between other stages
- Crawling – the baby moves purposefully towards the breast in search of the nipple
- Familiarisation – the baby familiarises themselves at the breast by licking, tasting, smelling and touching the nipple and areola area
- Suckling – the baby self-attaches at the breast and breastfeeding is initiated
- Sleeping – this is an involuntary activity of the baby around 1.5-2 hours after birth.
Six out of the nine stages (1, 3, 4, 6, 7, and 8) focus on activities of the newborn during the first hour of birth to propel themselves towards suckling needed for survival. The other stages (2, 5 and 9) involve distinct periods of rest. The baby uses all of its five senses on the way to the breast. This sensory information needs to be stored to become a memory. It’s thought that these rest periods are important to consolidate and strengthen the learning and memory of these new skills. This is why it is thought that self attachment during skin to skin aids the baby’s memory for future feeds.
It is therefore interesting to note that babies exposed to synthetic oxytocin during labour display fewer minutes of rest during skin to skin, significantly lowering their chance of suckling within the first hour, compared to babies who were not exposed.
This evidence is supported in the WHO/UNICEF Ten Steps to Successful Breastfeeding.
The Real Birth Company will launch a brand new induction of labour module in January 2025, which will be available to access within our digital antenatal workshop. We believe antenatal education is for everyone, and should cover all types of birth, regardless of an individual’s health picture. Providing information in this way creates greater knowledge, improved birth choice conversations leading to greater informed choice.




