
Induction of Labour and successful Breastfeeding
19 August 2024ICON – Supporting Parents to Cope with Infant Crying
25 September 2024
Sepsis Awareness Month
Each year the month of September marks Sepsis Awareness Month, with 13th September celebrated globally as World Sepsis Day. Individuals and organisations across the world come together to educate and inform about the importance of early recognition and timely treatment for sepsis.
According to the World Health Organization (WHO), maternal sepsis is the third most common cause of maternal mortality.
Maternal Sepsis Definition
Maternal sepsis is defined by the WHO as, “a life threatening condition that arises when the body’s response to infection causes injury to its own tissues and organs during pregnancy, childbirth, post-abortion, or in the immediate postpartum period”.
Sepsis can also cause complications following miscarriages as well as birth. The most common cause is a severe bacterial infection of the uterus or genital tract during pregnancy or immediately after birth, and can also be caused by a urinary tract infection (UTI) or pneumonia. Early diagnosis and prompt treatment is essential for improving perinatal outcomes following sepsis.
Neonatal Sepsis Definition
Neonatal sepsis is defined as sepsis which develops in infants in the first 28 days of life.
A Global Health Issue
Sepsis is a significant cause of maternal, neonatal and child mortality worldwide. Whilst the UK’s rates are significantly better than other low-middle income countries (1 per 100,000), maternal sepsis remains a leading cause of maternal death in the UK.
Improving sepsis outcomes within vulnerable populations (including pregnancy), will contribute to the achievement of a number of the United Nations Sustainable Development Goals (SDGs), including the target to markedly reduce global maternal and neonatal mortality rates by 2030.
Sepsis in Pregnancy
Pregnant women have a slightly higher chance of developing sepsis compared to the general population, due to naturally occurring changes that happen to the immune system during pregnancy, as well as the need for investigations, procedures and surgery. Other associated risks can also cause complications such as prolonged rupture of membranes (PROM) or gestational diabetes. Women with chronic health conditions affecting one or more of their organs, are also more susceptible to developing sepsis.
Sepsis can be harder to detect in the pregnant population. This is mainly due to the fact that the majority of pregnant people are young, fit and healthy, but also down to the natural adaptations of pregnancy. These factors can mask signs and symptoms of sepsis until the point where a patient is already very unwell. This is why the National Early Warning Score (NEWS) tool, used to improve the detection and response to deteriorating adult patients, should not be used for pregnant people; the Maternity Early Warning Score (MEWS) should be used instead. This is an adapted version of NEWS, specifically designed to protect pregnant mothers and their babies. The tool gives a better warning system to alert health care professionals when pregnant women become sick. The MEWS tool is currently being used extensively in maternity settings in the UK, but the aim is that every organisation will have implemented MEWS across England by March 2026.
“The new system will result in fewer false alarms and provide better care for mums and mums-to-be” – Maria Caulfield, Minister for Women’s Health Strategy.
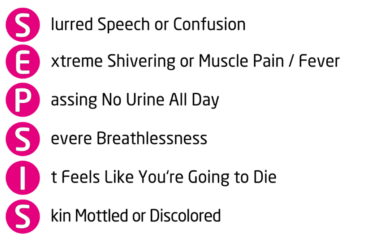
Think Sepsis! – How to Recognise Sepsis in Adults – The UK Sepsis Trust
Sepsis symptoms according to the Royal College of Obstetricians & Gynaecologists (RCOG):
● High or low temperature
● Tachycardia
● Tachypnoea
● Hypoxia
● Hypotension
● Minimal passing or urine
● Confusion or failure to respond to treatment
The RCOG also notes that these signs (including temperature) may or may not be present in someone with sepsis, and are not necessarily related to the severity of sepsis.
Factors that Increase Chance of Sepsis (RCOG):
● Obesity
● Impaired glucose tolerance/diabetes
● Impaired immunity/immunosuppressant medication
● Anaemia
● Vaginal discharge
● History of pelvic infection
● History of Group Beta Strep (GBS)
● Amniocentesis (or other invasive procedures)
● Cervical cerclage
● Prolonged rupture of membranes (PROM)
● Group A Streptococcus (GAS) infection in close contacts or family members
● Of black or other ethnic minority group origin
Maternal Sepsis Rates
Between 2006-2008 sepsis rose to be the leading cause of direct maternal deaths due to GAS infection, rising to a count of 13 women. These women died as a result of genital tract sepsis in pregnancy; 5 were related to pregnancy complications prior to 24 weeks of gestation, and 8 were related to sepsis from 24 weeks gestation, arising before or during labour. Sadly, substandard care was identified in many of these cases, particularly in the early recognition of the onset of sepsis, and a lack of guidelines on the investigation and management of genital tract sepsis were identified as part of the Confidential Enquiries into Maternal Deaths.
The 2009–2012 MBBRACE-UK (Mother & Babies: Reducing Risk through Audits and Confidential Enquiries Across the UK) Confidential Enquiry found that almost a quarter of the women who died had sepsis.
These cases prompted the need for a specific guideline on the management of sepsis in pregnancy, which now exists. The Confidential Enquiry at the time highlighted how early recognition, diagnosis and prompt treatment of sepsis is crucial for improving outcomes and mortality rates.
The latest MBBRACE-UK report, investigating maternal deaths in the UK between 2020-2022, found that after thrombosis, thromboembolism and COVID-19, the next most common direct causes of maternal death were suicide and sepsis due to pregnancy-related infections, which were responsible for the same number of deaths.
– Maternal sepsis causes 261,000 maternal deaths worldwide.
– The UK maternal sepsis mortality rate is 1 per 100,000.
– The United States has the third highest rate of maternal morbidity of all high income countries – between 2017-2019 14.3% of all pregnancy related deaths in the U.S were due to infection or sepsis.
– Recovery from sepsis is both physically and mentally challenging with 40% of people reporting cognitive and/or psychological after effects (The UK Sepsis Trust).
– Sepsis can affect milk production and the ability to breastfeed a baby – it may take months before an individual is well enough to do so.
– Severe sepsis with acute organ dysfunction has a mortality rate of 20-40%, which increases to 60% if septic shock develops.
Reducing Maternal Sepsis Rates
Sepsis is a life threatening condition which if left untreated, can lead to multiple organ dysfunction, septic shock and in severe cases, death. Maternal sepsis is also associated with an increased risk of newborn death by up to 10 times.
Like any form of sepsis, maternal sepsis can’t be prevented completely, but there are things that can be done to reduce the chances of developing an infection.
Promoting and practising good hand hygiene, for example, by washing hands thoroughly both before and after changing maternity pads or checking sutures.
Since pregnant women are also at a heightened risk of developing sepsis from other sources, including influenza, the ‘flu’ vaccine is recommended for pregnant women. Encouraging and promoting uptake of the influenza vaccination during pregnancy can also help reduce the chances of developing maternal sepsis. The flu vaccine is safe for pregnancy, offered annually throughout the winter months (September to March), and can be given from 12 weeks of pregnancy.
You can find more information on the flu vaccination here.
Moving Forward
Sepsis is a significant cause of maternal and perinatal morbidity and mortality around the world including in high-income countries. These figures stress the need for better recognition, early diagnosis and appropriate treatment of maternal sepsis, and the importance of introduction and implementation of guidelines and early warning trigger tools to better support pregnant mothers and their babies.




